Background to the research
When harmful microorganisms enter the body of a preterm baby, they can cause an infection. The body responds with inflammation as part of its immune defense but in preterm babies, this process can sometimes be more harmful than helpful.
In a healthy immune response, white blood cells, including T cells, detect the infection, become activated, multiply, and send signals to other cells to fight off the germs. Once the infection is gone, most of these T cells die, but some turn into memory T cells which help the immune system to react faster if the same infection happens again.
In preterm babies, the immune system does not always work properly. If T cells do not die off, or if they fail to become memory cells, the inflammation can continue longer than it should, leading to chronic inflammation. This ongoing inflammation can damage delicate brain tissue in preterm babies and may contribute to brain injury or developmental issues later on.
Why is this type of research important?
Finding a safe and effective way to treat inflammation and related health problems in preterm babies is an ongoing challenge. Within PREMSTEM, we are exploring the use of human mesenchymal stem cells (H-MSCs) as a potential solution.
These stem cells are special because they can help to control the activity of immune cells which play a key role in inflammation. In addition, H-MSCs have the ability to repair and regenerate tissue, making them a promising option for helping the body to resolve inflammation and prevent long-term brain damage.
What were the aims of the research?
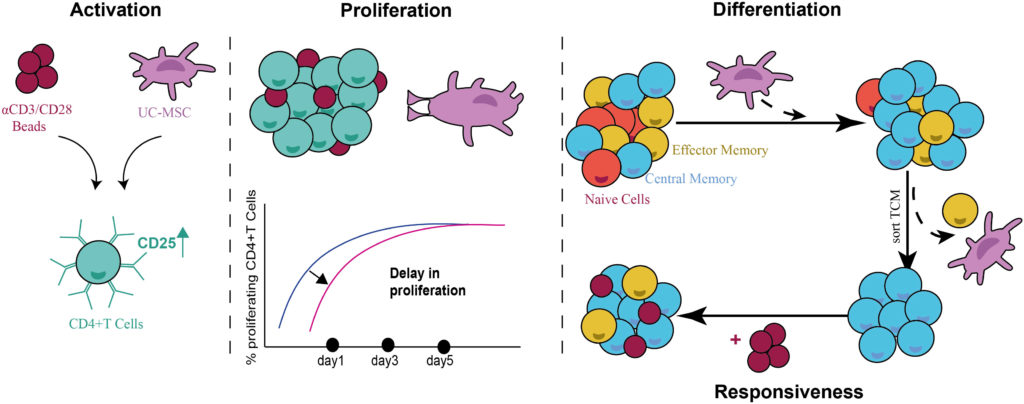
The goal of this study was to create a cell culture model to observe the long-term effects of H-MSCs on activated T cells. The researchers wanted to answer several key questions:
- Do T cells become memory cells when H-MSCs are present?
- How do H-MSCs affect the activation and multiplication of T cells?
- Can these newly formed memory T cells respond more quickly to the same type of infection if it happens again?
- How do H-MSCs control this process with T cells? Do they do it through direct contact between cells or by releasing signalling molecules?
By answering these questions, the researchers hoped to better understand how H-MSCs can influence the immune system and help manage inflammation, especially in vulnerable populations like preterm babies.
How was the research done?
In this study, T cells were activated using αCD3/CD28 beads to create an inflammatory response. Once activated, the T cells were placed with umbilical cord mesenchymal stem cells (UC-MSCs) and the researchers looked at how the UC-MSCs affected the T cells under four different conditions:
- Indirect cell contact: The UC-MSCs and T cells were grown in separate compartments so that they didn’t touch but could still share nutrients and signals through a tiny filter.
- Direct cell contact: The T cells and UC-MSCs were allowed to touch each other directly.
- Support medium: A growth solution for the UC-MSCs was added to the T cells.
- Blocking proteins: The proteins made by either the T cells or UC-MSCs were blocked to see if this changed the results.
In all of the conditions, the researchers measured how the T cells reacted including how they multiplied, how they became memory cells, how they responded to a second encounter with the same stimulus, and what proteins they produced. These conditions helped the researchers to understand how UC-MSCs might influence the immune response, especially in controlling inflammation.
What did the research show?
In this study, the researchers found that:
- UC-MSCs helped create more memory T cells when they were cultured together.
- The T cells stayed active in the presence of UC-MSCs, but they multiplied at a slower rate.
- The memory T cells responded to a second encounter with the same stimulus (the αCD3/CD28 beads).
- The strongest effect of UC-MSCs on T cells happened when the cells were in direct contact and when UC-MSCs released certain proteins.
- Two proteins, IL-6 and TGF-β, seemed to play a role in how UC-MSCs affected T cells but more research is needed to understand this better.
These results suggest that UC-MSCs could help control inflammation and immune responses, possibly offering a way to improve the body’s healing processes.