Our research explained
Why do we use animals in our research?
overview
Babies born preterm are extremely fragile because many of their body functions and vital organs are not yet sufficiently developed. As a result of preterm birth, they often develop brain damage which can affect the way that they think, learn or move throughout their whole life.
Our project is working towards showing that a stem cell therapy can be used to treat brain injury in preterm born babies to improve their quality of life as they grow up.
As a research team we need to demonstrate that our cell therapy is safe and effective before we can test the stem cell therapy in preterm babies. The complexity of the brain and the complicated interactions between the organs in our body make it impossible to predict how any stem cell therapy will work using computer models.
To make sure that any new therapy is safe and ‘does the job’ we use animal models to see how it works in a living organism. Furthermore, it is a legal requirement to carry out sufficient laboratory studies and tests on animals before seeking approval for human studies.

What are ‘animal models’ and why do we use them in our research?
Animal experiments allow researchers to test theories about how a disease develops or how a new drug might react in different scenarios. In this project we will use animal models to recreate the impairment occurring in the preterm brain and test drugs to see how they work to protect the brain cells. We will be able to test different variables in a controlled setting.
Although similar to us, tests in animals cannot fully predict how a therapy will work in humans. Once we have convincingly shown that our stem cells can repair the brain in animals and have no serious side effects, the next step is to test our cell therapy in babies.
How have animal tests already helped to improve healthcare for babies?
Studies in sheep models have led to the discovery and implementation of various medical treatments which have drastically improved the survival of preterm born infants.
Studies using sheep models have shown that therapeutic hypothermia (a type of treatment to lower the body temperature) can prevent damage from birth asphyxia (a condition arising when the body is deprived of oxygen) in term infants.
Thanks to such tests in animal models, antenatal steroids (given to pregnant women expecting preterm delivery), surfactant therapy (to support a baby with its breathing) and hypothermia are now standard treatment methods for vulnerable newborns, and these interventions have helped to significantly improve infant survival and wellbeing.

What is the '3R' principle?
To protect the wellbeing of our research animals we will follow the 3R principle outlined as follows:
- Replacement: Animal experiments will be replaced with alternatives whenever possible.
- Reduction: Only the minimum number of animals required for statistical analysis of results will be used in order to reach valid conclusions without the use of excessive animals.
- Refinement: Suffering of animals will be avoided or kept to a minimum. Experiments in live animals will be performed in accordance with the European Community guidelines for the care and use of laboratory animals.
The 3R principle makes our approach to animal testing more responsible. By following the 3R principle, we will only use as many animals as is necessary to collect our data and avoid distress to animals as far as possible.
As a collective, the PREMSTEM team includes neonatal intensive care specialists, paediatricians, and obstetricians with vast experience running clinical trials. In this project we will rigorously address all ethical, legal, social and safety issues associated with our research activities under the guidance of an Ethics Advisory Board.
What animal studies are we planning?
We will test our cell therapy in five small animal models (rodents) and two large animal models (sheep) of preterm brain injury.
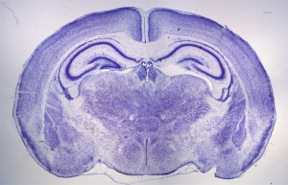
Rodent models
The research we conduct in rodents is very valuable. As they are small and easy to work with, we will be able to screen our cell therapy in multiple experiments and refine our tests before moving to the large animal model. Our rodent studies will therefore minimise the research we need to do in sheep.
Sheep models
The sheep brain is very similar in overall structure to the human brain. Like us, sheep also have a long pregnancy during which the baby's brain grows a lot. Rodents on the other hand have a short pregnancy and the brain normally develops after birth – this is why we will also test the therapy in sheep. These tests will provide comparisons with most of the brain injury types seen in preterm born infants and produce the data and understanding we need to design clinical trials in preterm babies.
In conclusion, the research we conduct in the lab with animal models will help us to understand the best way to use the stem cells to treat brain injury in preterm infants. These investigations will help us to design effective clinical trials in babies and ultimately provide an accessible and effective therapy to repair brain damage common in preterm infants – a treatment option not currently available.