Background to the research
Brain injury in babies, known as neonatal encephalopathy, disrupts essential developmental processes that are needed for the brain to function properly, such as the development of nerve cells (neurons) and their connections.
Hypoxia-ischemia is a type of brain injury that happens when a baby’s brain doesn’t receive enough oxygen (hypoxia) or blood flow (ischemia) at the end of a pregnancy and/or around the time of giving birth. It can cause long-term disability such as problems with the capacity to learn and think, the ability to move and perform everyday tasks like walking or riding a bike, or eyesight deficits.
The standard therapy for this kind of brain injury is to cool down the whole body using hypothermia treatment within the first six hours after birth. However, 40–50% of babies who receive this cooling treatment will still suffer from major neurological problems.
Scientific studies have been showing the promise of stem cells to treat brain injuries. Stem cells have the special ability to self-renew (make more stem cells), become other types of cells in the body, and release growth factors which have positive effects on injured tissue.
Why is this type of research important?
There are still many things about stem cells that we don’t understand, such as the role of extracellular vesicles which come from mesenchymal stem cells, a type of stem cell found in various tissues including the umbilical cord and bone marrow or fat. Extracellular vesicles are involved in transportation and communication between cells, carrying proteins and other compounds from one cell and delivering them to another.
Scientists think that stem cells achieve most of their therapeutic effects thanks to extracellular vesicles, making them a potential alternative to cell therapy. However, we still only have limited data demonstrating the protective effect that they can have.
This study is an important step in better understanding how extracellular vesicles can reduce inflammation in brain injury in both adults and babies, and how they protect the brain from apoptosis (death of neurons) and loss of brain tissue.
What were the aims of the research?
The research aimed to discover the effect of extracellular vesicles from mesenchymal stem cells on tissue and cells in a brain injured by hypoxia-ischemia. Previous studies have looked at the effect of extracellular vesicles from mesenchymal stem cells within the first few hours after brain injury develops. In this study, the researchers wanted to see their impact at a later phase of the injury – equivalent to several months to a year old in humans.
How was the research done?
This research used mice to test an animal model of hypoxia-ischemia in newborns. Typically mice are used in research because of their similarity to humans in terms of bodily structure (anatomy) and functions (physiology) and genetics.
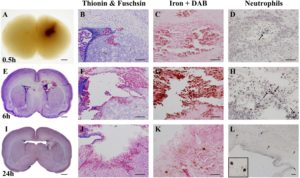
To bring about hypoxia-ischemia, the researchers reduced the blood and oxygen flow to the brain by restricting the main artery in the body which delivers blood to the head and neck. The mice then spent one hour in a low oxygen environment.
On three different days after the brain injury developed, the scientists injected the treatment (the extracellular vesicles from mesenchymal stem cells) into the animals and one week later, started to assess the effect that the extracellular vesicles had on the injured brain.
Three groups of animals were included in the study:
- The control animals received no extracellular vesicles.
- The test group received extracellular vesicles from mesenchymal stem cells where the stem cells had been cultured in a special solution containing nutrients called human platelet lysate, a solution to get the stem cells to grow, made up of platelets from blood donors.
- To provide a comparison, the third group received extracellular vesicles from the same solution but without stem cells to find out what effect the culture itself was having on the brain injury.
The researchers first checked for cell loss and death in the brain’s tissues and cells and looked for changes in the size of the brain, in particular to see if it had got smaller (brain atrophy). To do so, they rated nine different regions of the brain, giving each one a score between 0 and 3 depending on the amount of cell loss or damage that they saw. They looked for atrophy by measuring the volume of both sides of the brain and using staining techniques to observe different features.
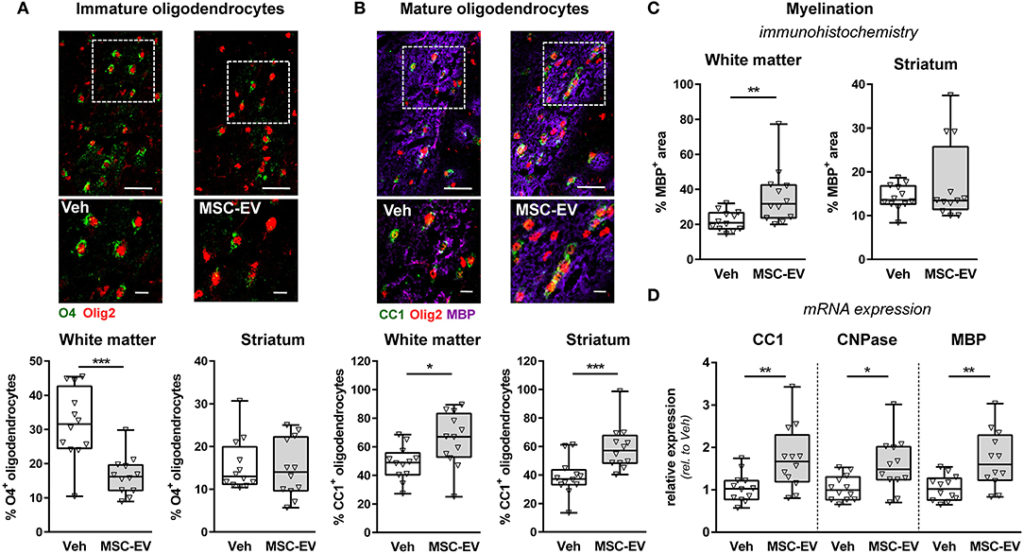
To study the effect of the extracellular vesicles from mesenchymal stem cells on different cells in the brain such as neurons (nerve cells), the research team used cell markers and labelling to track if and how the treatment had affected cell growth, cell density and the cells’ ability to perform important functions like developing connections between neurons.
What did the research show?
The results of this study suggest that extracellular vesicles from mesenchymal stem cells increase the survival rate of neurons and/or promote neurogenesis (the process of forming new neurons) by controlling the responses of microglia (a type of cell that supports immune responses and remodelling) and astrocytes (a type of cell that supports maintenance/function). These brain cells can sometimes make injury worse by causing inflammation.
The study also suggested that extracellular vesicles from mesenchymal stem cells promote important processes in the developing brain, such as myelination, a process of wrapping neuron axons with myelin to help neurons to send messages around the body.
The team also demonstrated that the protective and supportive effects they saw were from the extracellular vesicles from mesenchymal stem cells rather than just the extracellular vesicles found in the special solution used in the third group of mice.
They were able to partially confirm findings from other models of brain injury which may provide a clearer focus for future studies. However, they also noted the difficulty in directly comparing results between studies because of inconsistencies and differences in stem cell donor/cultivation or the preparation of extracellular vesicles.
This study has contributed important new information to the field, showing that a therapy using extracellular vesicles from mesenchymal stem cells can be used within a delayed therapeutic window (the timeframe when a treatment’s effective) and could potentially be combined with hypothermia treatment to improve outcomes for patients with brain injury.