Our research explained
Neonatal encephalopathy
What is neonatal encephalopathy? What triggers it?
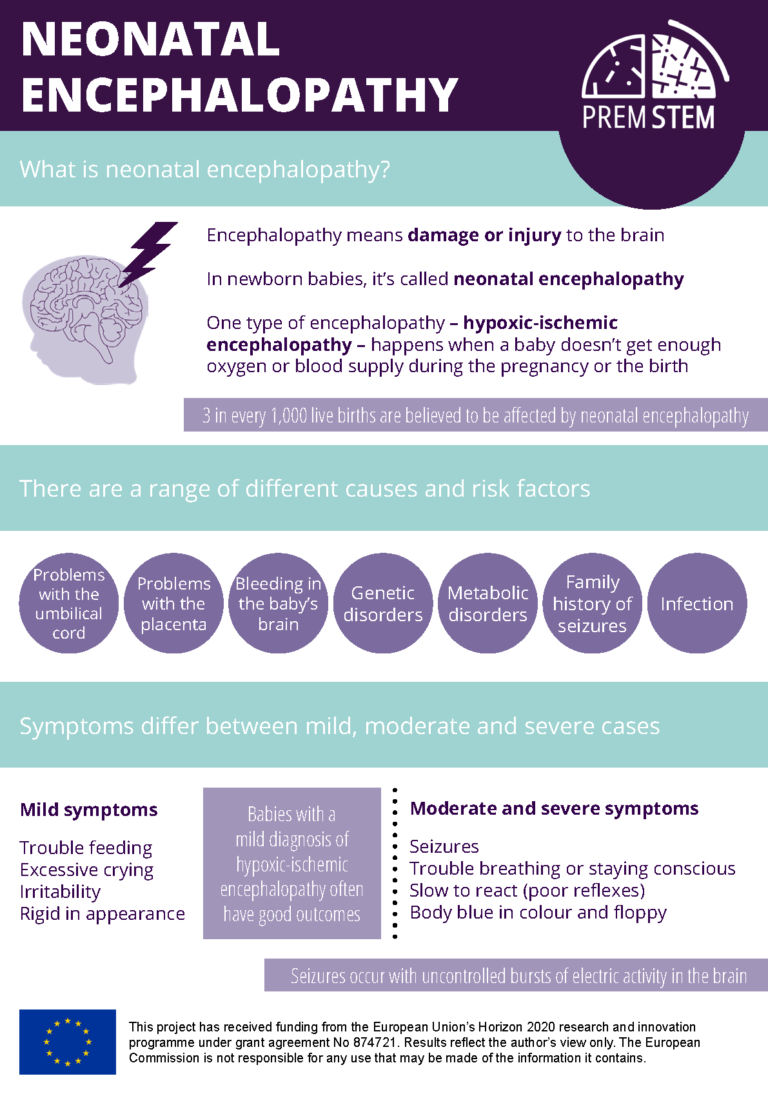
Encephalopathy means damage or injury to the brain. When it happens to a newborn baby, we call it neonatal encephalopathy. There are a few types of encephalopathy, including hypoxic-ischemic encephalopathy which occurs when a baby doesn’t get enough oxygen or blood supply during the pregnancy or the birth itself.
A mild case of hypoxia limits the growth of cells in the body, but a case of severe, acute hypoxia means cell death. Furthermore, the ischemia (lack of blood flow) not only contributes to the low oxygen supply but means the foetus is not receiving the glucose (energy) needed by cells to survive.
What are the risk factors and causes of neonatal encephalopathy?
Neonatal encephalopathy can be caused by a range of different reasons, including problems with the umbilical cord or placenta possibly linked to infections (e.g., in the uterus), bleeding in the baby’s brain, genetic and metabolic disorders, or a family history of seizures.
Restrictions in oxygen or blood flow to the brain (hypoxia-ischemia) are the most common cause of neonatal encephalopathy. However, the medical team most often won’t be able to tell which of all these possible causes has led to an individual case of brain injury.
How is neonatal encephalopathy diagnosed?
Signs of neonatal encephalopathy can already be picked up soon after birth, for example during the baby’s Apgar test done by medical staff one minute and five minutes after they’re born. This test measures the infant’s:
- Appearance (skin colour)
- Pulse (heart rate)
- Grimace response or reflexes (the baby’s reaction to a light pinch)
- Activity (muscle tone)
- Respiration (breathing rate and effort)
Another test which may help to detect neonatal encephalopathy looks at acid levels in the baby’s blood in their first hours of life (lactic acidosis). In the womb, ischemia (lack of blood flow) can prevent the placenta from removing waste products such as carbon dioxide and will increase acidity levels in the body, including in the blood.

How do you know if your baby has encephalopathy?
Three in 1,000 live births are believed to be affected by neonatal encephalopathy.
A baby with mild neonatal encephalopathy may have trouble feeding, cry excessively, be irritable, or appear rigid. In moderate and severe cases of neonatal encephalopathy a baby may have seizures, have trouble breathing or staying conscious and be slow to react (have poor reflexes). They may physically look blue in colour and appear to be floppy (lacking muscle tone).
How is neonatal encephalopathy treated? Is a there a cure? What is cooling treatment for newborns?
Hypoxic-ischemic encephalopathy is the only type of neonatal encephalopathy that has an approved treatment, which is to cool the baby’s body down using hypothermia or cooling therapy. Babies suffering from hypoxia may seem like they’re doing fine for several hours after birth – this is because in this time of stress, the individual cells of the brain are using all their energy reserves to survive.
After six hours, the cells’ energy reserves run out and symptoms of encephalopathy begin to show. For example, it takes a lot of energy for the brain to keep neurons under control or ‘on standby’ until they’re needed to send signals. When the brain’s energy supply runs out, the neurons ‘switch on’ and can cause an uncontrolled burst of electric activity in the brain. This causes seizures, which are one of the signs of brain injury.

For this reason, it’s important to start therapeutic hypothermia in the six-hour window after birth for it to have the most positive impact. Lowering the baby’s body temperature to 33.5°c slows down the various processes taking place within the cells of the body – including those which are going wrong – and reduces inflammation in the brain. Research shows evidence that this cooling technique increases the survival of neurons (nerve cells) and limits damaging effects caused by overactivated immune cells.
Babies usually receive therapeutic hypothermia for three days. To see how the baby reacts to the treatment, the medical team will carefully monitor the baby’s brain activity and be on guard for any other problems which can happen with hypoxic-ischemic encephalopathy, such as bleeding on the brain and stroke. Scanning techniques such as ultrasound and MRI are used to look at any damage inside the brain.
These babies may also need help with their breathing using a ventilator or treatment for seizures. Seizures are caused by unusual bursts of activity between the neurons in the brain when they don’t have enough energy to control their own behaviour.
Therapeutic hypothermia is offered to babies with moderate to severe hypoxic-ischemic encephalopathy. Babies with a mild diagnosis of hypoxic-ischemic encephalopathy often have good outcomes (there are babies who will recover fully) and do not undergo this treatment, as the risks outweigh the benefits, as some babies who receive it will need sedatives or be at increased risk of heart, gut or blood clotting issues.

How long can a baby live with encephalopathy?
Some babies do not survive neonatal encephalopathy. For those that do, their outlook depends on the severity of the brain injury – whether mild, moderate, or severe. Many babies diagnosed with moderate to severe neonatal encephalopathy are at risk of some form of lifelong change linked to their brain injury, for example in terms of memory, movement, or learning.
How long does it take to recover from encephalopathy?
Babies with mild neonatal encephalopathy may recover fully and have no long-term problems.
Moderate or severe cases of neonatal encephalopathy can lead to certain difficulties which will affect the rest of the baby’s life. These can include cerebral palsy, epilepsy, behavioural disorders, or problems with learning, speech, or hearing.

Cerebral palsy
Researchers at our partner the Cerebral Palsy Alliance are investigating a prevention and cure for cerebral palsy, a physical disability caused by injury to the developing brain that affects movement and posture.

How is PREMSTEM providing hope to babies with neonatal encephalopathy?
Research projects like PREMSTEM are contributing to our knowledge about stem cells and their potential to treat encephalopathy. PREMSTEM is researching a treatment to improve brain damage in preterm born babies, which is known as encephalopathy of prematurity. You can read more about preterm birth and brain injury in our fact sheet. The lessons learnt and knowledge from PREMSTEM will benefit all babies in the long-term.
Below are other examples of how our partners are contributing to scientific knowledge which may one day help to treat babies with neonatal encephalopathy.

Stem cells and exosomes
Researchers at the University of Gothenburg are part of the scientific community looking at the possibility of using stem cells, perhaps in combination with therapeutic hypothermia, to treat encephalopathy in term babies. They’re looking at exosomes – balloon-shaped sacs that form on the side of cells – which are constantly released by stem cells. The active components of exosomes are the growth factors and molecules found inside the sacs. Research is showing that exosomes, like their stem cell big brothers, may have a positive effect on brain injury.
Ultrafast ultrasound
Iconeus is developing improved scanning techniques using ultrafast ultrasound to allow the clinician to see inside the brain in more detail and at a higher resolution to the technology we currently use. Being a mobile device, they’ll be able to use it directly at the cot side. This will help with the diagnosis of the brain injury and help to monitor improvements following hypothermia treatment. This is important for ensuring that babies with neonatal encephalopathy receive the targeted and specialist support that they need after they have left hospital.